What is OCD?
The acronym OCD stands for Obsessive compulsive Disorders. It comprises of two distinct clinical presentations i.e. obsessions and compulsions. It has a prevalence rate of around 3% in the general population. The World Health Organization has placed OCD as one of the top 10 leading causes of disability in the developed world.
The typical features of Obsessions and compulsions are described as under
OBSESSIONS: These are certain patterns of thoughts which are:
-
Ideas, images, impulses, memories etc
-
intrusive, repetitive, and anxiety provoking
-
considered as absurd and irrational by the clients themselves and they are unable to control them.
-
these thoughts are recognised as individual’s own thoughts even though they occur without individual’s will
-
these are recognised by the sufferer as repugnant or unacceptable in nature.
COMPULSION: These are certain behaviour patterns which are:
- repetitive, ritualistic
- unpleasant to the individual carrying them out.
- these behaviours are carried out with the objective of undoing an obsession, at times in a magical way.
- the individual views them as pointless and makes an effort to stop them without success.
Common obsessions and compulsions:
-
Fear of contamination: This is the most common obsession encountered where the person has a fear of getting contaminated by dirt or germs. This results in undue emphasis on cleanliness – the person indulges in washing rituals, avoiding dirt prone areas all the time etc.
-
Doubting: Preoccupation with thought that one has not completed a task successfully eg hurt someone whilst driving. This results in compulsive behaviour of checking that no harm has occurred, the doors are locked, gas knobs are switched off, etc. This stems from one’s childhood when they fail to receive clear messages or approval from their parents, and as a result of this they are not sure if they have done the right thing. Such obsessive and compulsive behaviours are often associated with feelings of low self-esteem or guilt.
-
Fear of illness, germs, or bodily fear: Fear of getting infected by agents like microbes/virus, this too may result in washing and avoidance behaviours
-
Symmetry: There is an urge to arrange the items in a symmetry and keeping things in order. Some OCD clients indulge in elaborate night-time rituals before going to bed which can involve – organising things in a meticulous and orderly manner, repeating certain words or phrases a certain number of times. There may be a counting ritual to keep a track of the activities involved.
-
Sexual or aggressive thoughts: Some patients report having blasphemous thoughts or images which may be highly distressing. At times clients report that certain songs from radio or television get stuck in their mind and they can’t free themselves from them.
-
Magical thinking: Few patients specially children and adolescents perform certain behaviours in order to undo an underlying fear of dangerous things happening to them or to their near ones. Avoiding stepping on intersections of tiles on floor can be a symbolic attempt to avert danger to their family.
| ICD-10 diagnostic guidelines:
The following symptoms must be present for at least two weeks and be a source of distress or interference with activities. a. They must be recognised as the individual’s own thoughts b. There must be at least one thought or act that is still resisted unsuccessfully, even though others may be present which the sufferer no longer resists. c. The thought of carrying out the act must not in itself be pleasurable – simple relief of tension or anxiety is not regarded as pleasure in this sense. d. The thought, images, or impulses must be unpleasantly repetitive. |
What is the cause of OCD?
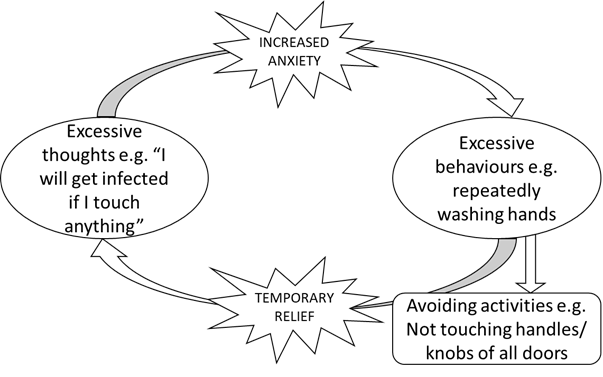
The Behavioural model states that previously benign/neutral thoughts after being repeatedly associated with Anxious state becomes an OBSESSION. Gradually these thoughts get triggered easily and become intrusive. As a protective response to this the mind operates various attempts to decrease the built anxiety which maybe in the form of avoiding those triggers or performing actions intended to decrease the anxiety associated. These responses are called COMPULSIONS. This temporary decrease in the anxiety prevents the normal habituation of anxiety and thus reinforcing the behaviour in future whenever any stimulus is encountered. A typical cycle of thoughts and action in OCD illustrated in the diagram below:
 The brain areas that are involved in this process are the ones responsible for filtering the external stimulus and preventing unnecessary responses by the brain namely the Cortico‐striatal‐thalamo‐cortical (CSTC) circuit. The cycle of obsessions and compulsions when repeated several times lead to long term changes in the brain and strengthens this and other related neural circuits. This process has been implicated in development of the disease.
The brain areas that are involved in this process are the ones responsible for filtering the external stimulus and preventing unnecessary responses by the brain namely the Cortico‐striatal‐thalamo‐cortical (CSTC) circuit. The cycle of obsessions and compulsions when repeated several times lead to long term changes in the brain and strengthens this and other related neural circuits. This process has been implicated in development of the disease.
Is OCD genetic ?
Many factors have been implicated in the development of OCD but no single factor is yet proven to be always present. Environment factors like being raised in a religious background or parents having strict cleanliness in house may lead to OCD. Although it is known that the first-degree relatives of patients have a slightly higher than normal risk of OCD than general population but the association is not certain.
Is OCD a psychotic disorder?
Sometimes they may appear similar to psychotic experiences in terms of their senselessness and bizarreness, but the difference here is that in the case of obsessions the person has a good insight into the abnormal nature of these thoughts. There is an element of magical thinking in obsessions that lead to compulsive behaviour. About two to seven percent of OCD clients go on to develop psychotic symptoms.
Is OCD an impulse control disorder?
No; Compulsions are different from impulse control disorder in that in compulsions the person is forced to carry out the actions they don’t like, whereas in impulse control disorder the activities carried out are inherently pleasant such as gambling, drug and sexual addictions etc to the person.
Is OCD a part of Depression?
The relationship between OCD and depression is complex. There are cases when Obsessive and compulsive symptoms may appear in the presentation of a depressive disorder while on the other hand many patients suffering from OCD may have clinical depression or depressive symptoms secondary to OCD. It can be ascertained mainly by the onset – which came first. The severity of symptoms would be another indicator as to which of the two disorders is primary.
Is there a treatment for OCD?
There are many treatment options for OCD. Usually a multimodal treatment is planned for the patients which includes psychological interventions, social interventions, and drug treatment.
CBT – Exposure with response prevention therapy (ERP) and sometimes Cognitive behavioural therapy (CBT) is mainly indicated in most patients as a part of psychological intervention. ERP has two components i.e. EXPOSURE to the anxiety provoking stimuli in a gradual manner and RESPONSE PREVENTION of the protective responses to break the reinforcing cycle.
The type of exposures can be real-life, imaginal, or virtual in nature depending on the situation. After repetition, the patients gradually learn that the anxiety subsides on its own and they develop tolerance to the physiological effects of anxiety. Eventually there is a recognition that these protective behaviours are redundant, and patient decreases the repetitive behaviours. It is also observed that therapy sessions lead to changes in the brain leading to long-term response. For example, symptom provocation in OCD leads to increased regional cerebral blood flow (rCBF) in the right caudate along with some other parts of the brain. After psychotherapy in the form of CBT, this activity reduces, which correlates with the degree of improvement in symptoms.
When a person experiences obsessive thoughts of contamination associated with a particular stimulus, say being near a toilet seat or touching it, he or she may do a repetitive behaviour of repeated hand washing to get relief from the anxiety associated with obsessive thoughts. This relief reinforces environmental triggers, for example, experiencing obsessive thoughts even when looking at the toilet seat, or looking at its picture or even thinking about it and thoughts of someone else using it. The person then eventually starts performing compulsive acts in all such situations to get relief from the anxiety.
Drug Treatment:
Antidepressants are the mainstay of treatment for OCD. Drugs like fluoxetine, sertraline, and Clomipramine are commonly used. It is seen that almost 50-70% patients respond well to treatment. Sometimes antipsychotics such as olanzapine or aripiprazole or addition of a 2nd antidepressants such as venlafaxine or mirtazapine may be necessary to achieve response. It is also important to get treatment for any co-occurring psychiatric or medical illness. In very few resistant cases other modalities like transcranial magnetic stimulation, or electroconvulsive therapy.
Am I too late for treatment?
Patients with OCD usually seek treatment after 10-15 years. Common factors associated with treatment delay are many. Initially many patients think that their behaviours are normal part of their personality and will fade away with time. Some symptoms are also not considered absurd by family members. There might be shame and because of which people hide their symptoms. Few individuals may just have a trait of perfectionism which is a characteristic of OCD prone personalities. Indecisiveness and slowness are another hallmarks of OCD behaviours. There might be a fear of taking psychiatric medication or treatment. Usually earlier the treatment the better the chances of getting better.
Where should I seek help from?
If you or your dear ones are having symptoms mentioned above with significant distress or problems in carrying normal activities, you should consult your Psychiatrist immediately. The psychiatrist will evaluate thoroughly the symptoms of OCD, whether you require treatment or not and order any investigations if required.
After relevant examination the decision to treat on Out-patient basis or in-patient basis will be taken. The situations where a psychiatric admission may be indicated are – if the patient has high suicidal risk, is unable to take adequate self-care, is danger to others, there is a need for intensive therapy, or if there are any medical/psychiatric complications.
Recommended Reading
-
Veale D, Willson R. Overcoming Obsessive Compulsive Disorder: A self-help guide using cognitive behavioural techniques. Hachette UK; 2009.
-
International OCD Foundation | Homepage. Available from: https://iocdf.org/
